Children are not just “little adults” and should not be assessed as miniature versions of an older population. While episodes of lower back pain throughout adulthood is relatively common, it is less frequent in children. As well, children are more likely to have a more specific cause of symptoms than adults, particularly if symptoms persist beyond the norm.
There seems to be a combination of factors that predispose a young person to an injury of their spine, including behavioural, genetic, and mechanical features. Currently, it is thought that a combination of repetitive stresses and sports that require hyperextension movements can predispose young athletes to higher rates of injury, but this is difficult to specifically determine between sports. Maturity of different parts of the spine develop between 10-15 years of age, which can vary significantly between children, who are usually grouped by age in sport and activity. Up to half of young athletes that experience an extended bout of lower back pain may have the beginnings of a stress fracture.
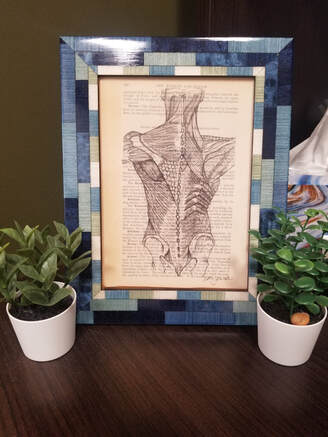
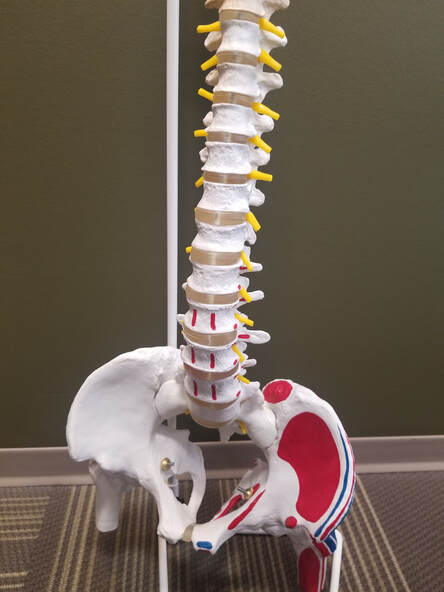
Spondylolysis (Stress Fracture) is one of the most common causes of persistent lower back pain in children and adolescent populations. Particularly in those that are engaged in active sport. It most commonly occurs at the bottom of the lower back in the bone that meets up next to the pelvis. This seems to be due, in part, to the fact that the bones are still developing and have not achieved their full density or strength, which continues to increase well into adulthood.
When assessed, the symptoms will likely worsen with back-bending/extension or with repeated movements. There are rarely neurological symptoms like numbness, tingling, or weakness. If there are any nerve-type symptoms or positive tests, it may warrant different tests or considerations be made for their treatment.
If stress fracture is found in the early stage, it can heal in approximately 90% of patients in about 3 months.
It is important to listen to young people who are experiencing their pain. Asking open-ended questions and getting the history of what they have been experiencing. While some young people are more forthcoming than others, they have the best information available as the person experiencing their pain/symptoms.
Observation of the affected area, active range of motion, passive range of motion, muscle testing, joint mobility testing, and neurological screening are all included in a good examination of the concerns. If there is no suspicion of more serious issues, imaging is often not required. However, this requires a thorough history and examination to make the best clinical decision. If the assessment and history are suspicious of a bone injury though, a series of x-rays can be very valuable for determining if further action is required.
Even if they are not an athlete, if their symptoms fit with the clinical examination of a spinal injury, they should be considered for treatment and further imaging. Warning flags such as participation in contact sports, nerve symptoms, and unrelenting back pain could not always predict if x-ray changes would be found, but early imaging is recommended due to the increased risk for athletes in these age groups.
Conservative treatment (non-surgical) is the first step in management as most patients have excellent outcomes and surgery is rarely necessary. Treatment such as activity modification, exercise and functional rehabilitation can all play a role in someone’s recovery.
The vast majority of cases can be treated successfully with non-surgical means. If a stress fracture or bony injury is found incidentally or without symptoms, no further treatment is typically required. The common goal if a symptomatic stress fracture is found is to allow the bone to heal, but even in fractures that do not come back together fully on x-ray the outcomes are still generally positive.
While there is no need to scare anyone when experiencing pain or symptoms, it is important that we listen and make sure that we are providing support to younger people who may struggle to articulate or advocate for themselves. If there are any questions about this or any other information, please feel free to reach out to the office.
- Trent, PT
Linton, A.A., Hsu, W.K. A Review of Treatment for Acute and Chronic Pars Fractures in the Lumbar Spine. Current Review in Musculoskeletal Medicine (2022) 15:259-271.
Schroeder, G.D. et al. The role of intense athletic activity on structural lumbar abnormalities in adolescent patients with symptomatic low back pain. Eur Spine J (2016) 25:2842-2848.
Pate, JW., et al. Assessing a child or adolescent with low back pain is different to assessing an adult with low back pain. J Paediatr Child Health. 2022 APr; 58(4):566-571.
Sairyo, K. et al. A review of the pathomechanism of forward slippage in pediatric spondylolysis: The Tokushima theory of growth plate slippage. J. Med. Invest. 62:11-18, February, 2015.



 RSS Feed
RSS Feed