Between 1984 and 1991, breast cancer was on the rise in Canada. We saw an increase in numbers with the advent of mammography in the early 1990’s, followed by a slight decrease in around 2002 with a decrease in prescription of hormone replacement therapy.
Thankfully, we have seen a steady decline in mortality rates from breast cancer since 1986.
This is due to
- improved screening,
- earlier diagnoses and
- improved treatments for this pathology.
Surprisingly, evidence of breast cancer rehabilitation as far as I can gather, only really just began around 2005. Between 2005 and 2009, less than 15% of patients with breast cancer participated in any form of rehab program.
A 2019 study by Sciliba et al. concluded the following:
“The current model of care for women with breast cancer focuses mostly on treatment of disease; this approach too often lacks attention to patients’ physical and functional well-being.” Many criticisms emerge from this review.
We suggest that there is a need to strengthen the level of evidence for many commonly used clinical practices and to better describe innovative rehabilitative approaches.”
While this is not overly surprising as treatment for diseases in general focuses on the medical treatment, and much less on restoring the function and well-being of the patient.
Enter physiotherapists! We became a profession post World War II, to help rehabilitate amputees and wounded soldiers in hospital. Of course, since then we have grown in both scope and numbers to optimize people’s function and well-being after illness and injury in all aspects of human health. So why not breast cancer too?!
The treatment and rehabilitation of women diagnosed with breast cancer has grown and evolved especially over the last 17 years and continues to do so. As a profession we have much to contribute and can play a major role in optimizing quality of life during and after diagnosis.
Once diagnosed, the first order of business is to develop a plan for medical treatment.
This will vary and is based on
- type of carcinoma,
- stage of disease (usually categorized from stage I-IV) and other factors such as co-existing comorbidity(ies),
- age etc.
This therefore may or may not include:
- surgery (lumpectomy or mastectomy +/- lymph node removal +/- breast reconstruction);
- radiation and/or chemotherapy or just radiation or just chemotherapy;
- pharmaceutical and/or hormone based therapy.
- Reduced strength of the upper extremity
- Reduced shoulder mobility
- Scar tightness (breast and/or axilla)
- Upper extremity ache or pain
- Lymphedema of the upper extremity
- Neuropathic pain
- Musculoskeletal pain (breast, axilla, and/or neck-shoulder)
- Chronic pain
- the patient’s subjective report, clinical history followed by
- an objective examination of the neck, shoulder, elbow, wrist and hand joints, upper extremity strength, upper quadrant mobility and muscle tone,
- scar assessment, and
- neurological function of the upper extremity nerves.
Together with the patient and based on both the subjective and objective examinations, an individualized plan is developed to target the identified symptoms and impairments to optimize function and quality of life. The plan can include the following:
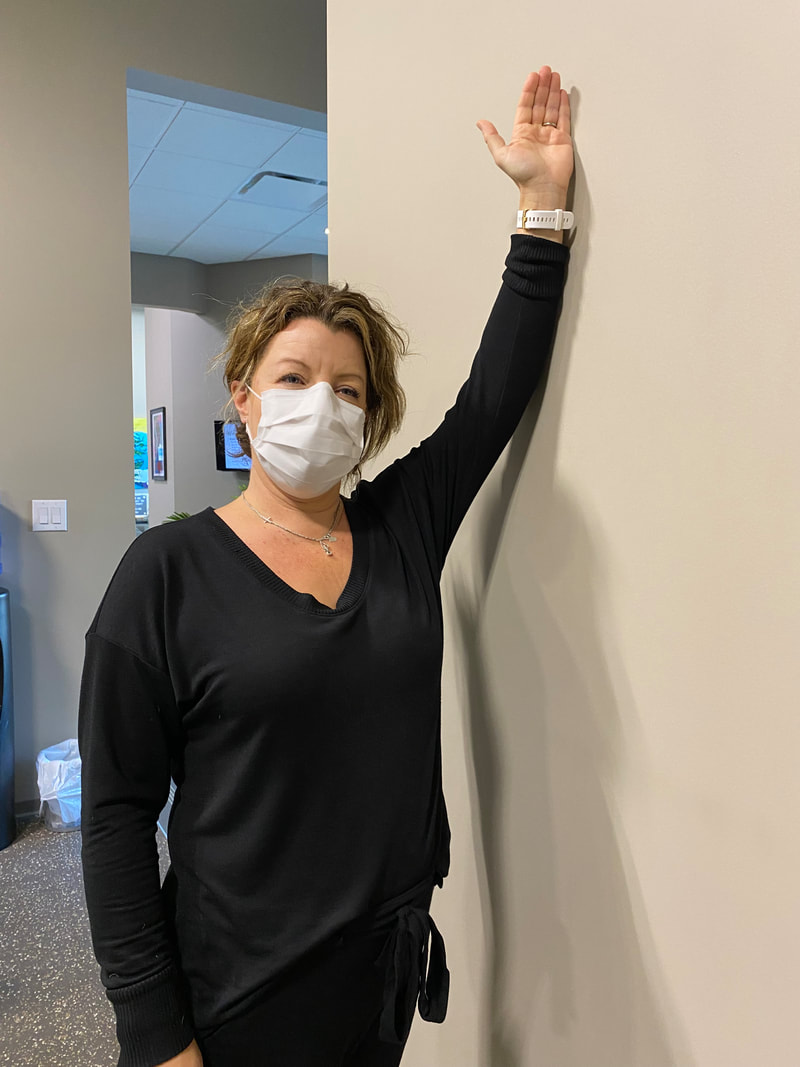
- Range of motion and stretching exercises to improve mobility restrictions related to the soft tissue and scar extensibility.
- Manual therapy such as joint mobilisation, myofascial release and neural tension reducing techniques.
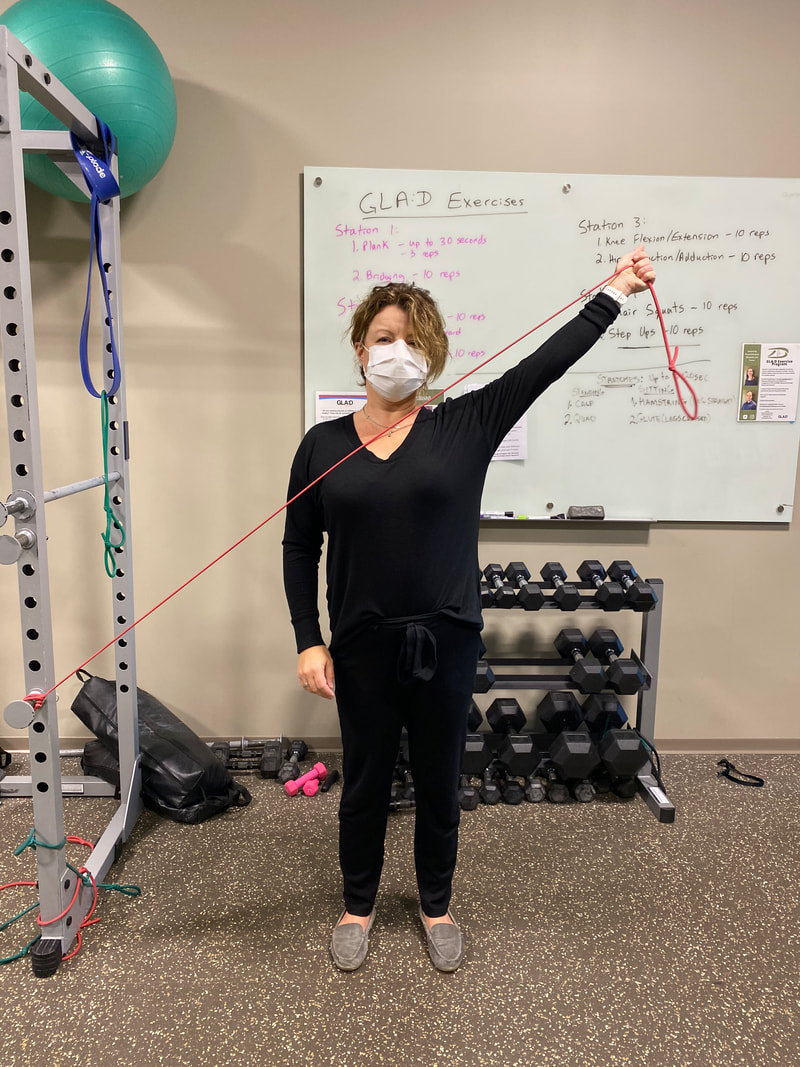
- An aerobic and strengthening exercise program, usually with bands to start, to strengthen the upper quadrant muscle groups, postural and core stabilizers.
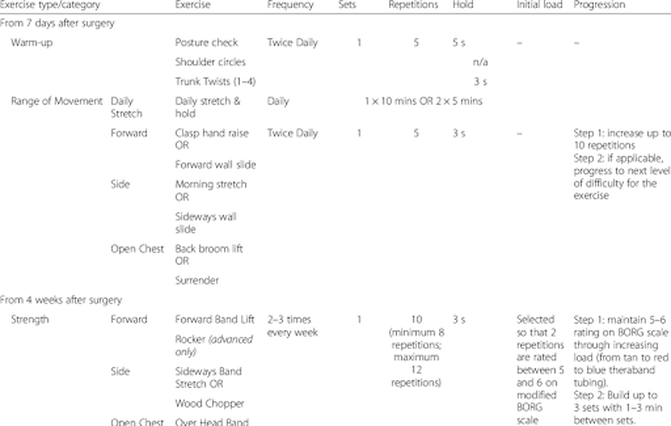
The literature identifies a structured program called PROSPER (Prevention of Shoulder Problems Trial) that is introduced at one week post-operatively, improved upper extremity function and arm symptoms including pain as well as quality of life at one year post non-reconstructive surgery. Some exercises are pictured below!
Lymphdema refers to localized swelling of the body caused by an abnormal accumulation of lymph. Post-surgical breast cancer patients can experience edema in the upper extremity which can cause pain/discomfort, decreased mobility of the arm, and compromise circulatory and nerve function in the arm.
There are several types of lymphedema:
- A mild type of lymphedema can occur within a few days after surgery and usually lasts a short time.
- Lymphedema can also occur about 4 to 6 weeks after surgery or radiation and then go away over time.
- The most common type of lymphedema is painless and may slowly develop 18 to 24 months or more after surgery. It does not get better without treatment.
Treatment of Lymphedema:
- Exercise. Exercise helps improve lymph drainage. Specific exercises will be advised by your doctor or physical therapist.
- Bandages. Wearing a compression sleeve or elastic bandage may help to move fluid, and prevent the buildup of fluid.
- Diet and weight management. Eating a healthy diet and controlling body weight is an important part of treatment.
- Keeping the arm raised. Raising the arm above the level of the heart when possible lets gravity help drain the fluid.
- Preventing infection. It’s important to protect the skin in the affected area from drying, cracking, infection and skin breakdown. Your healthcare provider will advise you about how to care for your skin and nails to help prevent problems.
- Massage therapy. Massage by someone trained in lymphedema treatment can help move fluid out of the swollen area.
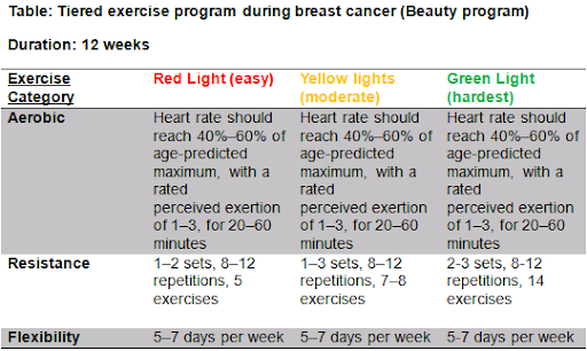
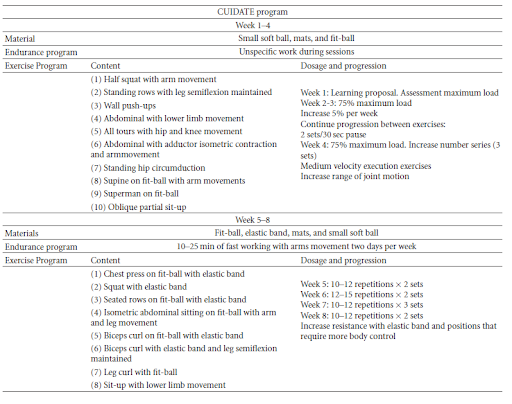
The literature indicates relatively low compliance with exercise in breast cancer patients. This is despite the well known physical and psychological benefits of a physical conditioning program. In order to counteract concerns such as fatigue, quality of life, social anxiety and overall deconditioning, the BEAUTY program is a recommended tool to guide frequency, intensity, time relative to the type of exercise. See chart below.
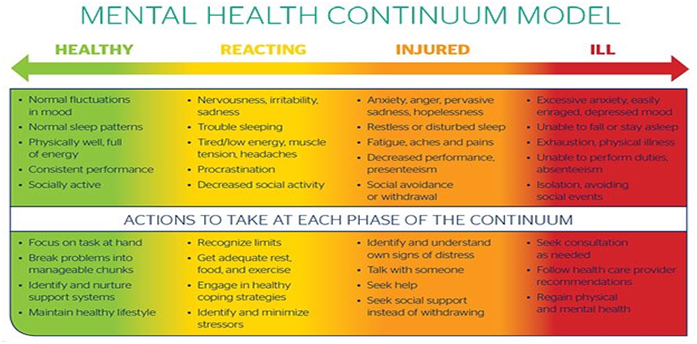
Education is a key component of physiotherapy treatment. Using the biopsychocial model of health, a physiotherapist can help identify the needs of the patient, offer both manual treatment as well as psychological support. Furthermore, this approach to health not only serves the patient best but allows the physiotherapist to act as a liaison with members of the interdisciplinary team.
Additionally, physiotherapists are well equipped to create and direct a plan to assist the patient in returning to work and normal activities of daily living. This can include work site assessment, functional conditioning program and return to work planning.
Take Home Message:
So the take home message is simply that physiotherapists are well equipped to help patients diagnosed with breast cancer. They can help improve symptoms, mobility, strength, thereby empowering patients to improve their quality of life by returning to their hobbies and leisure activities, activities of daily living and so much more.
If you or someone you love has been diagnosed with breast cancer, get them to a physiotherapist ASAP! There is no time like the present to be better and do better than we did yesterday!
Want to learn a bit more - join me for the Webinar on Wednesday October 26 @1pm! Just click below!


















 RSS Feed
RSS Feed